This month marks three years since the COVID-19 pandemic irrevocably changed the health care landscape. On March 13, 2020, Gov. Greg Abbott declared a state of disaster for all Texas counties. Schools went online, Texans were urged to stay at home and hospitals paused elective procedures.
The world stopped and waited for an end that took years to arrive.
The effects of the pandemic were felt most acutely by those working in health care. Since March 2020, hospitals have contended with ever-evolving guidance, surges and a pervasive workforce shortage that requires hospitals to do more with less.
The one constant over the past three years is the heroism of our hospitals and health care workers. As cases climbed, Texas hospitals shined, and our state’s health care heroes continue to scrub in and care for patients.
Heroes Work Here
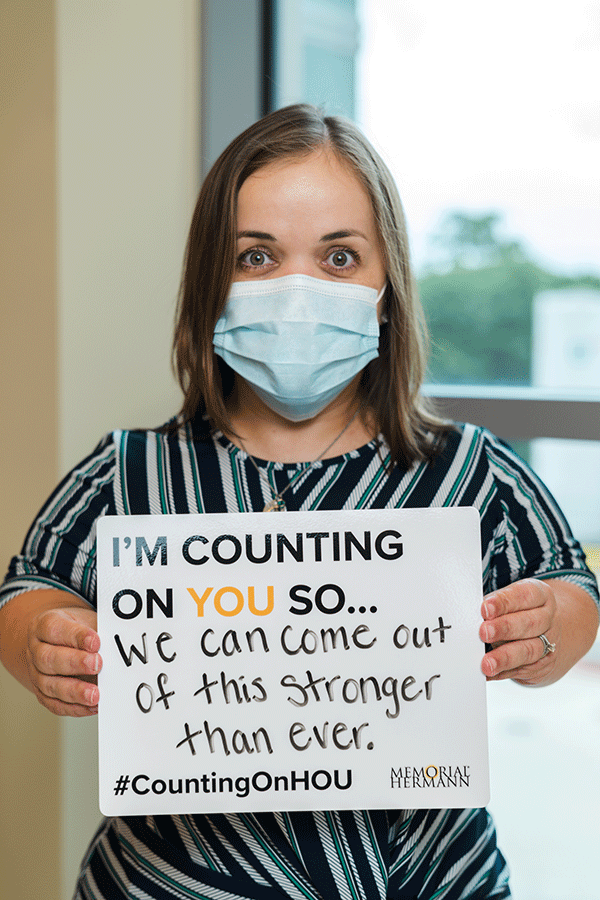
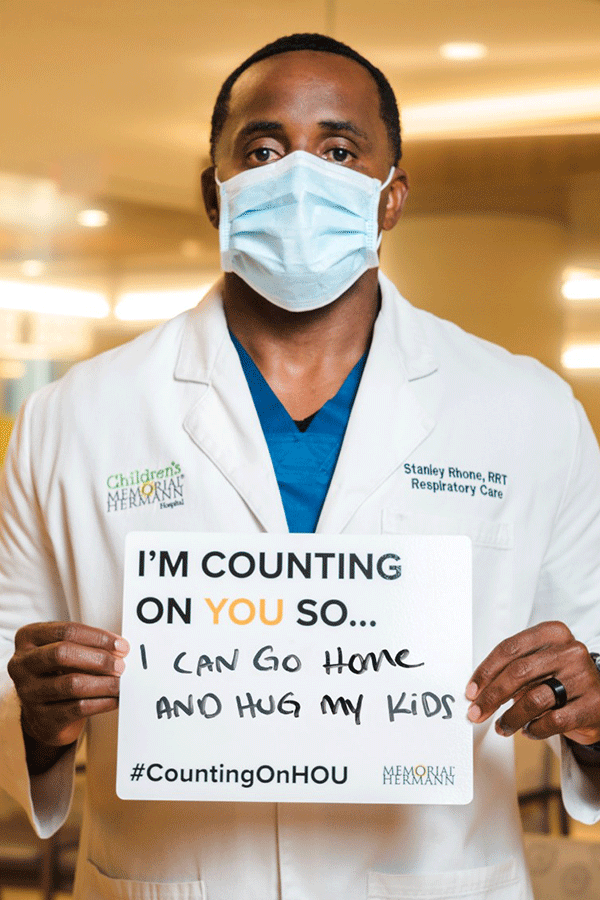
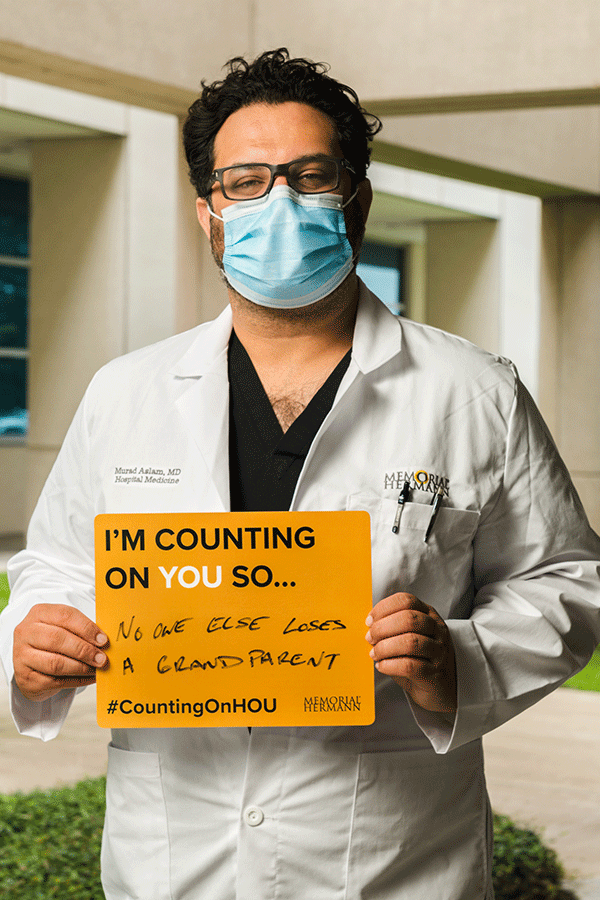
In the early days of the pandemic, photos of health care workers holding signs that said, “We came to work for you. Please stay home for us,” flooded social media feeds and “Heroes Work Here” signage adorned hospital lawns. The public’s heightened awareness of the health care workforce prompted hospitals to use social media to encourage the public to support frontline workers and adhere to preventative measures out of care for them.


Memorial Hermann’s CountingOnHOU campaign featured Memorial Hermann employees and affiliate physicians who reminded the Houston community of the importance of basic safety measures like wearing a mask, hand washing and maintaining social distancing.
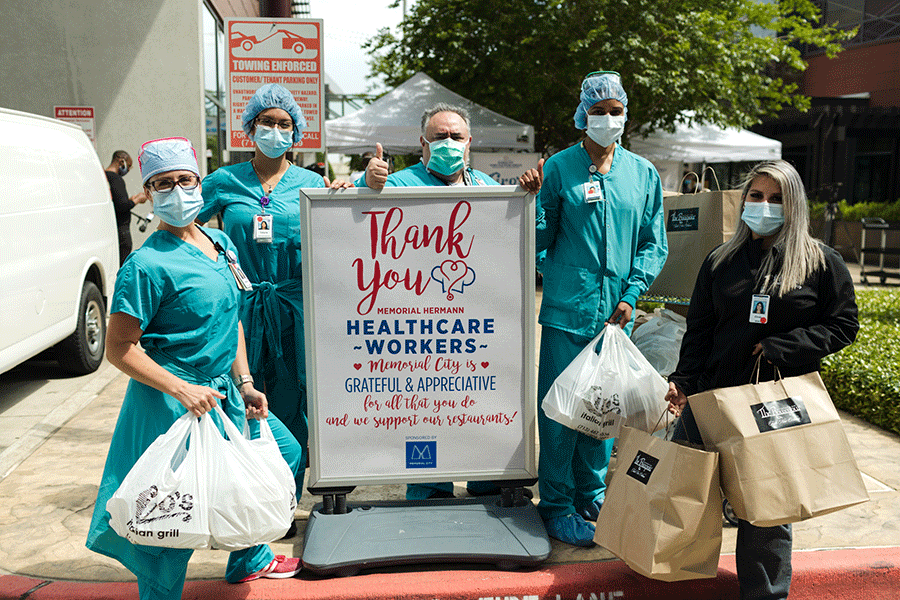
Frontline health care workers needed support and stability during this time of upheaval. During surges, many hospital workers had longer shifts and had less time to shop for groceries or pick up their children from school. To help their staff, several Texas hospitals implemented employee support programs to fill in the gaps.
To help hospital staff keep food on the table amid long shifts, worsened by inconsistent grocery store hours and supply chain disruptions, Harris Health offered pre-packaged produce bags that employees could preorder and pick up at the end of their shift.

To show appreciation for its employees and affiliated physicians, the Memorial Hermann Foundation launched “Feeding Frontline Families,” a program that encouraged community members to gift warm meals for health care workers and their families. The effort also encouraged community-support of local restaurants that were also experiencing financial strain due to the pandemic.

With in-person school and daycare suspended, the pandemic put many working parents in a challenging situation, especially frontline health care workers. UMC Health System partnered with the Lubbock Independent School System to provide childcare for the kids of hospital employees for 12 weeks. Tight safety protocols – such as masks, temperature checks and regular hand washing – were followed to ensure the program stayed virus-free.
Vaccinating Texas
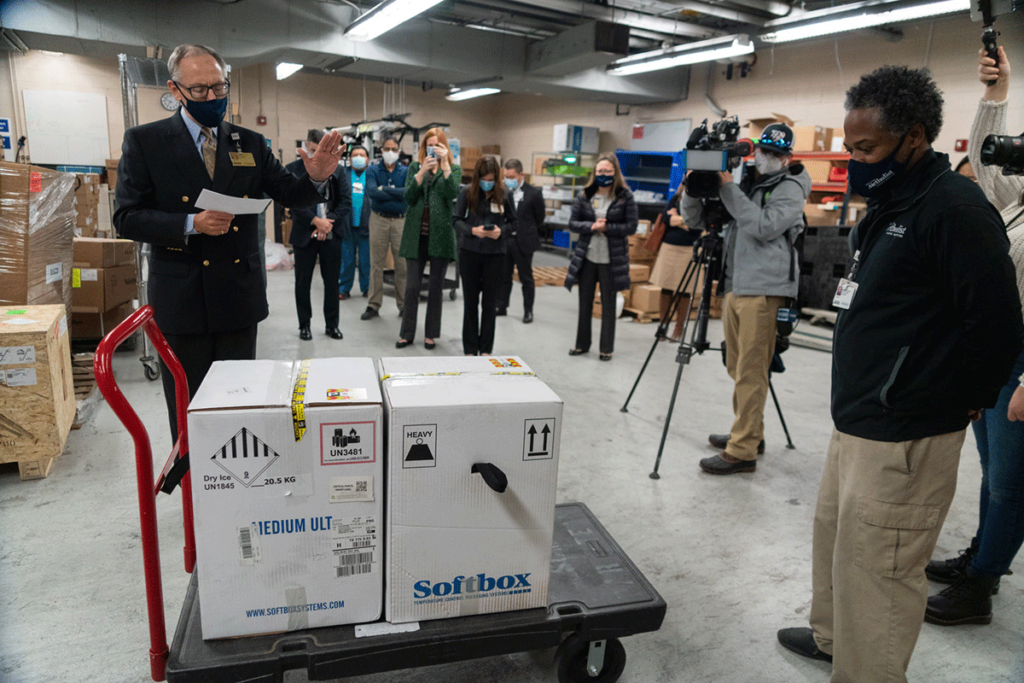
On Dec. 14, 2020, the first shipments of Pfizer’s COVID-19 vaccine arrived at Texas hospitals. Within the week, nearly a quarter million doses were distributed to 109 hospitals for “first tier” recipients, which included frontline health care workers. For them, the boxes of vaccines were the first sign of hope against a virus that, at the time, claimed the lives of 24,000 Texans and stretched the hospital workforce to unsustainable limits.

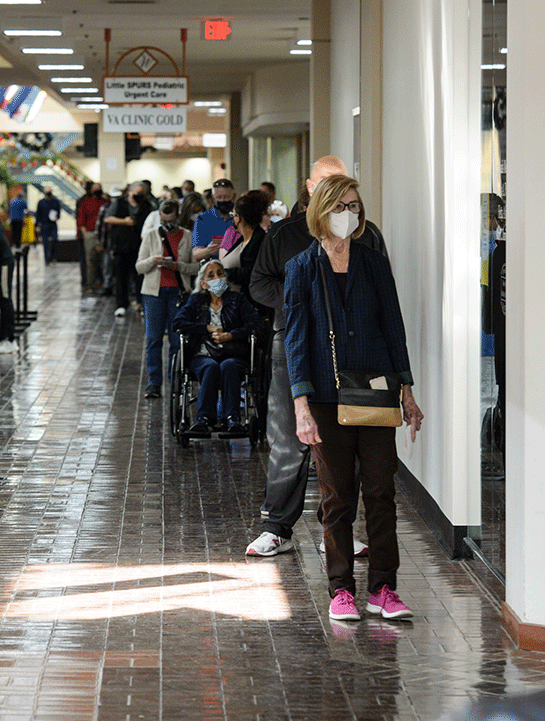
As the vaccine rollout progressed, the call to “get shots in arms” was dutifully answered by Texas hospitals. In January 2021, when vaccine eligibility expanded beyond the first tier of recipients, the need for large vaccine hubs became apparent.
In the spring of 2021, there were over 70 vaccine hubs in Texas – approximately half of them were managed by Texas hospitals and health systems. Vaccine providers had to contend with the appreciable challenges of operationalizing a large clinic that processed patients quickly, which included securing a large venue, staffing it and developing an automated system to register patients.

In January 2021, Memorial Hermann hosted the first of several mass vaccination clinics, where approximately 14,500 community members were vaccinated in just four days. The drive-through clinics were staffed and made possible by hundreds of volunteers from the community and from the health system. Part of what contributed to the success of Memorial Hermann’s vaccine hub was the development of a homegrown web tool as part of the registration process, which eliminated much of the required paperwork and allowed for each participant to be automatically integrated into Memorial Hermann’s electronic medical records.


When the FDA authorized vaccines for the public, a unique University Health multidisciplinary team came together to make them available. They stood up and operated one of the first and largest vaccination centers in Texas at Wonderland of the Americas, a centrally located shopping mall in San Antonio. The integrated team also routinely delivered vaccines to people in cars outside the mall entrance, and they took doses on the road to the homes of people who were homebound. At its peak, the Wonderland vaccination team was providing thousands of shots a day, with an all-time high of 8,000 doses in a single day. By the end, they had delivered 495,788 doses of COVID-19 vaccine.

In May 2021, the biennial revenue estimate was increased by $1.67 billion, moving the state from a negative to a positive balance. Texas Comptroller Glenn Hegar credited the improvement to the state’s successful mass COVID-19 vaccination efforts. Despite its challenges, the vaccine rollout was memorable for patients and providers alike. For vaccine recipients, getting the shot symbolized protection. For vaccine providers, giving the shot to thousands of patients every day is a tangibly gratifying experience for those who’ve dedicated their careers to caring for others.
Transforming Health Care Delivery
From infection prevention to telemedicine, the pandemic dramatically changed health care access and delivery. As hospitals looked to reserve beds, resources and staff for surges, patients embraced staying at home. They opted for more remote health care, including options for care that otherwise would only have been available within a hospital.
The share of Medicare visits conducted through telehealth, skyrocketed from approximately 840,000 in 2019 to 52.7 million in 2020, according to a December 2021 report from the US Department of Health & Human Services.
Not only did shelter at home orders make home care a more attractive choice, but access and reimbursement for telehealth services was expanded.
In the early days of the pandemic, Baylor Scott & White Health was able to quickly leverage its digital health platform. Through MyBSWHealth, Baylor Scott & White became one of the first health systems in the nation to mobilize a COVID-19 screening and drive-thru testing effort for everyone who needed it.

Expanding its service to the community, Baylor Scott & White launched a unique COVID-19 remote monitoring program through the MyBSWHealth app. To date, the program has supported more than 170,000 adult and pediatric patients with mild illness while in quarantine. Once the COVID vaccine became available, MyBSWHealth enabled patients to schedule their COVID vaccine and boosters. To date, more than 368,000 vaccine appointments have been scheduled via MyBSWHealth.
Now, the MyBSWHealth app provides access to virtual health care 24/7, even to patients who do not have an established relationship with Baylor Scott & White.
The Next Three Years
2020 proved to be an epoch that will forever change health care delivery. Telemedicine, health care equity, staff retention and burnout have been re-examined more scrupulously with a post-pandemic perspective.
The effects of the pandemic will ripple throughout the health care industry for many years. In a recent survey of member hospitals, over 60% of the 178 hospitals that participated indicated a significant nursing shortage that disrupted health care delivery.
A separate report compiled by Kaufman Hall revealed the devastating financial impact the pandemic had on Texas hospitals. Nearly half of hospitals operated at negative margins in 2022, according to the report; expenses ballooned by more than $33 billion over pre-pandemic levels; and the number of hospitals at risk of closure nearly doubled compared to 2020, with almost one in 10 hospitals at risk of closure. It’s an untenable situation for hospitals and health care workers.
The events of the past three years heavily influenced THA’s policy priorities for the 88th Texas Legislature. Now, 10 weeks into the legislative session, THA is pushing hard to refortify the depleted health care workforce, address the growing need for behavioral health care and protect access to health care for rural Texans because the hospitals that were ground zero amid the pandemic deserve protection and support.
Legislation that’s passed by Sine Die will determine what the next two to three years look like for Texas hospitals. Stay up to date with THA’s Cap Recap, a weekly digest of the most hospital-relevant news under the Pink Dome in Austin.
