Talk to Frank Beaman about the latest legislative push to eliminate the way hospital clinics pay for just about every facet of their operation, and it doesn’t take much to get him riled up on the topic.
Beaman is the CEO of Faith Community Hospital in Jacksboro, one of hundreds of hospitals and health systems serving rural areas in Texas. For the second straight state legislative session, the Capitol is playing host to a concerted push to ban or severely curb facility fees, which pay for literally everything at a hospital’s outpatient clinic except physician services.
Beaman stresses what the Texas Hospital Association has tried to communicate to lawmakers both before and during the current session: To the extent that an issue exists with facility fees appearing on a patient’s bill, it’s not a hospital issue. Hospitals need to recoup that revenue to survive.
In fact, it’s an insurance issue. And Beaman is bewildered as to why insurers – enjoying a well-documented era of financial windfall – need this sort of help from lawmakers.
“The insurance companies have full power to control this. They can deny it,” Beaman said. “What seems to be missing in this is, every provider that’s in-network has a contract. That contract dictates what they’re going to charge, and it dictates what they’re going to be paid, what’s allowable. If we throw something on a bill that’s not part of the allowable, it gets denied. The insurance company sure doesn’t need the Legislature to step in and protect them from me adding a fee on there.”
THA’s advocacy team is closely monitoring every facility fee-related bill filed during this session, and working with bill authors and other lawmakers to negotiate language that wouldn’t result in gutting clinics all over the state – an inevitable result of a broad ban.
“Where are those people going to go?”
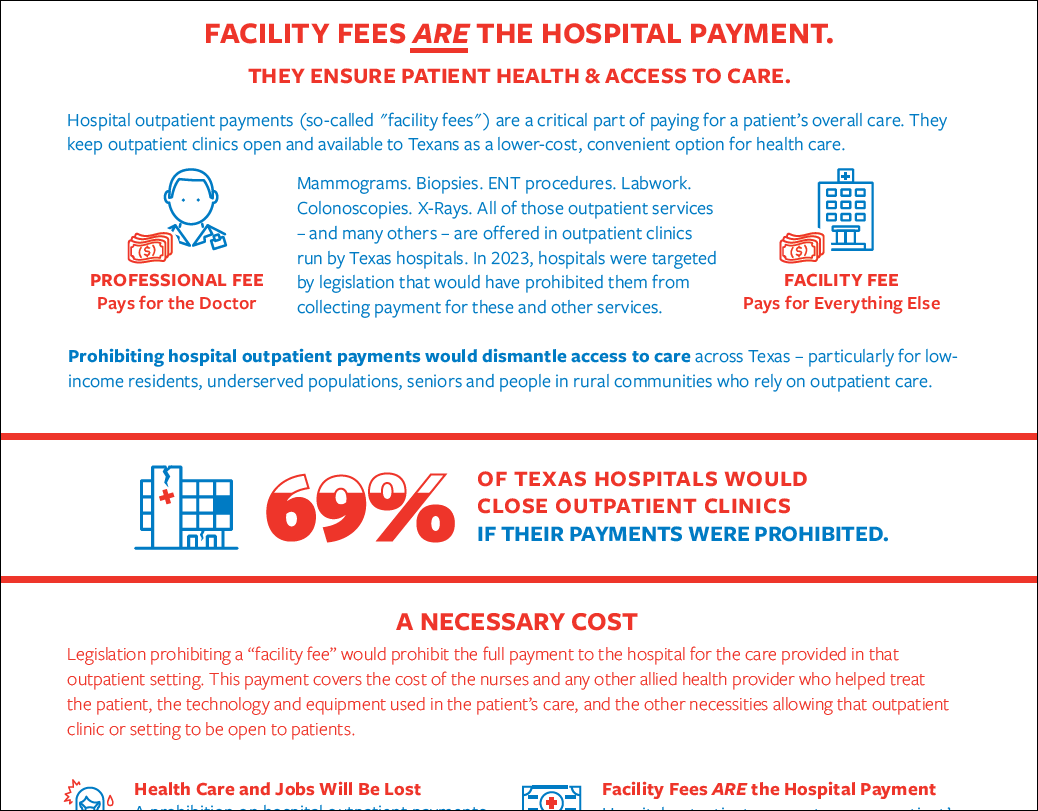
Contrary to the arcana that can send eyes spinning when someone looks over a detailed billing statement, the presence of a hospital outpatient department’s facility fee is simple both to explain and justify: A physician’s professional service fee pays for the doctor’s contribution to a patient’s treatment. The facility fee pays for everything else.
It’s truly that simple. Nurse pay, compensation for other medical and allied health professionals, lab technicians, hospital infrastructure, security, even the janitorial staff – all of it is covered by the facility fee. Without that all-encompassing coverage of expenses, hospital outpatient departments all over Texas would, at minimum, have to reduce service lines and staff.
In the worst case scenario, these clinics would have to close. And THA member survey results show these concerns are far from an outlier: In a 2022 survey on the impact of prohibiting hospital outpatient payments, almost 70% of respondents said they would have to close their outpatient clinic. Eighty percent said services would be reduced, and 85% forecast a reduction in staff if facility fees were prohibited.
That data helped THA make its case to successfully defeat several attempts to ban or restrict facility fees during the 2023 state legislative session. This time around, though, hospitals are facing similarly daunting legislative threats. One of the most problematic is House Bill 2075 by Rep. Tom Oliverson, MD (R-Cypress). As filed it would prohibit all facility fees except for care occurring on a hospital’s campus or for emergency care.
“That would simply be catastrophic for the industry,” said Sara González, THA’s vice president of advocacy and public policy. “We’re very willing to have a conversation about transparency, and making sure patients are informed of their choices, and can make those decisions on where they would like to seek care accordingly. But simply asking hospitals to provide services for free, that’s not a business model that anybody can really survive under.”
Working off the implications of HB 2075, Beaman says a ban on off-campus facility fees would affect three of Faith Community’s four rural clinics. Those three off-campus clinics are located in health professional shortage areas.
“So understand, we are now going to lose the ability to support a clinic in areas that are underserved,” Beaman said. “That’s an atrocious position to take, and why the Legislature would ever even consider that – but let’s just say they did. You’re talking about communities with a population of roughly, let’s just say 40,000 people in those particular areas. Those clinics see probably between … 40 to 50,000 visits per year combined.
“Where are those people going to go if we can’t support those clinics? That’s a big number. And it goes back to if you’re really concerned about the patients, let’s make sure they have access.”
Beating Back New Burdens
Another facility fee bill takes a less blanket approach, but would still represent a dramatic and detrimental change for hospitals all over Texas while introducing new administrative hassles.
As filed, House Bill 2556 by Rep. James Frank (R-Wichita Falls) and its companion, Senate Bill 1232 by Sen. Kelly Hancock (R-North Richland Hills), would prohibit facility fees for telehealth and “preventive care.” It also would require a national provider identifier (NPI) number for all providers and each provider-based facility they’re affiliated with. Every claim for a facility fee would have to include the unique NPI number for the facility where the patient received services.
“The biggest concern with [eliminating facility fees for] preventative services is that at the end of the day, it’s simply no payment for services that are really important for keeping the community healthy, keeping them out of hospitals,” González said. “And just from an access-to-care standpoint, those are services like colonoscopies, mammograms, well-woman health visits, well-child visits, etc. If a provider cannot be paid for those services, they will simply stop providing those services, and it will be harder for patients to get that care. It will also increase the cost of care, because we will now have fewer providers … in the system, which will just drive up the cost.”
Acquiring provider identifier numbers in the way the bill lays out would represent a new and unnecessary burden, González added: “The provision related to the unique NPI, that is a very big administrative lift for hospitals to implement a new NPI, and there are other existing channels that we feel would be less of an administrative lift, that we could do if the health plans want this information, we could do it in a less costly and less burdensome way.”
More information on the importance of facility fees is available in THA’s explainer, Texas: Don’t Dismantle Outpatient Care. The white paper notes that without these vital payments, vulnerable populations will be forced to seek care in emergency room settings; drive times and wait times for care will both increase as clinics close their doors; and costs will increase if patients can only receive specialized care in an inpatient setting.
Related articles from The Scope
THA’s 2025 Session in Review: Outcomes for Texas Hospitals
Medicaid talks in Washington, D.C., measles in West Texas and…
In a Unique Session, THA Survives and Thrives
There’s never been a legislative session quite like this one.…
2025 Legislative Session Recap: A Successful Juggling Act
Following the 2025 Texas Legislature’s adjournment sine die, Texas hospitals…
Congress Should Be Careful With Medicaid. Lives Are at Stake.
Since talk of a major congressional budget package began several…
National Hospital Week 2025: Appreciation and Awareness
National Hospital Week is a time to celebrate health care…
Texas Women – and Hospitals – Need the Certainty and Clarity of the Life of the Mother Act
There is nothing more central to the mission of a…