Rural Access is On the Ballot This November
With no major federal or state offices up for grabs, it’s likely most people aren’t thinking of this as an election year. But in fact, it is – and for health care champions, there’s one issue on the ballot particularly worth your participation, one that could potentially shape Texas’ health care landscape for a long time to come.
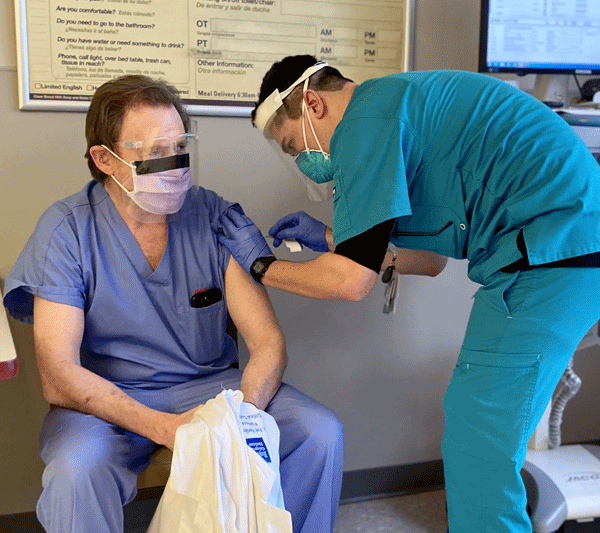
Let COVID’s Resurgence Be a Reminder: Get the Shots You Need
COVID-19 is back. And while it may not become a public health emergency this time – knock on wood – its resurgence serves as a timely note of caution.
Hard Work Continues on Behalf of Rural Hospitals
For some time, rural hospitals – the facilities in our state facing the greatest threat to their existence – have needed help. This year, in several key ways, the Texas Legislature provided a helping hand. But there remains work to do.
Hospitals Have New Hope to Regain Needed Personnel Power
For years, hospitals here in Texas have been experiencing that opposite: We’ve been hurting as our personnel numbers have waned. But now – after a legislative session in which the Texas Hospital Association stressed workforce again and again – we’ve got the barbells, bands and machinery to regain much of our lost strength.
Hospitals Survived a Siege This Session, and Look Now to Prevent Another One
Defense wins championships, the age-old expression goes in sports. Politics is sport in and of itself, and THA had to play some serious defense during the just-concluded session of the Texas Legislature. Now, the work begins to ensure that it doesn’t happen again.
Tell Congress to Keep Our Safety Net Wide and Strong
If there’s one theme you’ve seen me come back to in this column in the past year or so, it’s this one: Hospitals need help.
Vaccines Save Lives; Let’s Make Sure Texas Law Reflects That
It wasn’t long ago that that overwhelming numbers of people across Texas and the nation – on all sides of the political spectrum – knew and acknowledged that vaccines prevent diseases.
Managing Myths: The Facts About Texas Hospitals
An unfortunate reality in today’s world of fast-spreading information is, well, misinformation. With the internet and social media affording a potentially unvetted voice to just about everyone, misinformation is – ironically enough – a fact of life.
The Numbers Are In: Our Hospital Workforce Needs Serious Help
A recent Texas Hospital Association workforce survey reinforces and quantifies one fact that’s become abundantly clear: Hospitals are facing a breaking point for their workforce.
Work to Do in Washington: THA’s Federal Priorities
Earlier this month, the Texas Legislature gaveled in its 88th session, and what’s going on at our state Capitol will occupy a great deal of hospitals’ attention for the next four-plus months. If you’re a conscientious health care provider who wants the best possible care environment for your facility, city and state, I’m sure you’ll be following along, too.