The first image on the Texas Hospital Association’s (THA) internal site is a collage of staff portraits, a small but significant endeavor in measuring THA’s internal diversity, equity and inclusion progress, said Corey Cotton, Texas Hospital Association’s North Texas member ambassador. “Regardless of where we come from, this is who we are right now.”
Cotton heads THA’s internal committee for diversity, equity and inclusion, a group of twelve employees across THA’s family of companies. Created in 2020, Cotton said the group’s overarching task is to evaluate organizational efforts that promote diversity, equity and inclusion internally and externally, including identifying opportunities for staff development and best practices for an inclusive work environment.
“We created this internal committee because we understand that this is a forever project,” Cotton said.

“All of us at THA recognize the importance of cultivating a diverse, equitable and inclusive workplace. Achieving this environment is not a one-time commitment, but rather an ongoing project to ensure we’re doing everything we can to make everyone feel comfortable and valued,” said John Hawkins, president/CEO of the Texas Hospital Association.
After the prolific social justice movement in 2020, THA created an organizational committee comprised of executive leaders at member hospitals to identify and address the health disparities that exist in health care policies and practices. Since 2020, THA and Texas hospitals have worked to create equitable and safe workplaces, prioritize patient populations while delivering high-quality health care, and develop executive leaders that reflect the diversity of Texas.

“There are multiple layers to what hospitals have been thinking about,” said Jewel Mullen, M.D., MPH, associate dean for health equity at Dell Medical School in Austin, “The experience of the past two years, in particular, has pushed hospital leaders to think more deeply and expansively about what actions they need to take on behalf of their workforce.”
Shifting workplace culture and models to be more inclusive and equitable in Texas is a long-term and uncomfortable process, especially in the face of a national shortage of health care workers who provide care in these spaces. The past two years of the pandemic exacerbated the existing workforce shortages and contributed to provider attrition, so ensuring our health care workers are affirmed and supported in the workplace has become even more vital.
Texas hospitals rose to the challenge early in the COVID-19 pandemic by partnering with community organizations, addressing social determinants of health for their patient populations, and recruiting diverse employees, including at the executive level. Hospitals across the state worked to address health equity in their patient populations and diversity and inclusion in their organizations, increasing pressure on existing staff.
Now, diversity, equity and inclusion (DEI) leaders are working toward sustainable models to avoid getting burnt out.

“The challenge is how do you prioritize some of the things that you’re working on and prioritize what is going to be the best approach overall,” said Cotton.
Even before the pandemic, the nursing shortage was a problem in Texas. By 2032, Texas is expected to have a deficit of about 57,000 registered nurses and 12,500 licensed vocational nurses, with most demand coming from inpatient hospitals, nursing, and home health settings, according to a 2019 report from the Texas Center for Nursing Workforce Studies and Texas Department in State Health Services.
Dr. Mullen said this is why hospital and nursing leaders must invest in the professional development of nursing staff to simultaneously address workplace shortages and “to support educational pathways programs, to bring more people into the caring professions and to provide more support for people who want to move from the medical assistant or patient care technician roles into getting their LPN and their RN.”
At Dell Medical School, she said they are flexible to “create work conditions that suit people’s lives” to support their clinical work staff’s well-being.
Amid these structural labor pressures, Cotton said the THA’s DEI internal committee is committed to THA’s diversity statement, which guides both the internal and external DEI committees. “At THA, diversity means including all people, respecting their differences and valuing their viewpoints. THA is committed to an inclusive environment with varying perspectives that builds collaboration, innovation and productivity to better serve Texas hospitals. Diversity is important to the health care industry as it promotes quality care, understanding and respect.”
An anonymous survey that went out to about 80 internal THA employees made clear THA’s DEI priority areas: recruitment policies, alternative compliance hotlines, ensuring multilingual services, unconscious bias training, and ensuring all THA staff understand what diversity, equity and inclusion mean in the workplace.
Educational tools and DEI resources are one thing, but finding long-term solutions to cultivating more diverse, equitable and inclusive health systems in Texas is another. Cotton said the conversations around implementing DEI strategies, including tackling unconscious bias, have been difficult. But that is to be expected.
“I think anytime you get more than two people in the room and you’re having conversations about how to create change, there are all types of feelings involved,” he said.
Unconscious bias training and conversations should focus on interpersonal discrimination, but equally importantly, recognizing “how your implicit bias leads you to promote people who are like you,” said Dr. Mullen.
Marcos Pesquera is vice president for health equity, diversity, inclusion and community benefit at CHRISTUS Health System, headquartered in Irving, which reported in 2020 that 42% of their new executive hires the previous year were from racial/ethnic minority groups, surpassing their goal of 30%. He cited their partnerships with the National Association of Health Services Executives and the National Association of Latino Healthcare Executives, both organizations with missions to elevate the quality of health care services for historically marginalized and vulnerable communities.
Pesquera said their boards, providers, frontline staff, managers and directors are racially diverse, but “we have opportunities to diversify our Executive team.”
To address this, Pesquera said they recently started the Leadership Sponsorship Program, a program focused on developing minority director-level leaders. The primary goal is “closing the gap between the community, the diversity of the community and the diversity of our executive team.”
CHRISTUS executive sponsors who underwent training with Pesquera and his team are currently sponsoring four individuals. The sponsorship program includes regular meetings with fellows, quarterly leadership learning panels and shadowing of an executive sponsor.

“We have a coach assigned to the executive sponsors to help them grow and better relate to managers and directors or leaders who are different from them,” said Pesquera. They are also learning skills like inclusive language and checking for microaggressions.
“Those executives sponsoring are also getting help because we want them to truly connect with the individual and leave their biases behind.”
Dr. Mullen points out that when building models and strategies around anti-racism and inclusivity, it can be easy for leadership to turn to the same people who have “been bearing the responsibility for diversity and giving them the additional charge of improving the culture.”
“One has to think about the potential unintended consequences of saying that you are trying to support a more diverse workforce. You must be mindful of ways in which you might further burden that workforce by making them accountable for assuring inclusion and belonging. That responsibility starts with executive leadership,” said Dr. Mullen.
Pesquera admits that the movement and efforts around DEI, which evolved over the past two years, has been overwhelming. “We found ourselves taking care of fires.”
“You do training here, you an intervention there, you talk to people about this, you do an investigation there, and I’m not saying that it was excessive, but it was enough that you can exhaust any diversity practitioner.”
“We allocated time to sit down and plan a holistic approach to organize our interventions, and sometimes it is tempting to resort to multiple trainings without an overarching plan.” Pesquera said, “We identified DEI influencers across our organization and equipped them with skills to facilitate conversations across lines of differences in their areas. By working with smaller teams, we are slowly building capacity beyond our small department.”
Partnering with third parties such as human resources or patient engagement and outside resources, such as professional development coaches, the Catholic Health Association and the American Hospital Association, CMS office of Minority Health and others, has proven to be very helpful, Pesquera stated.
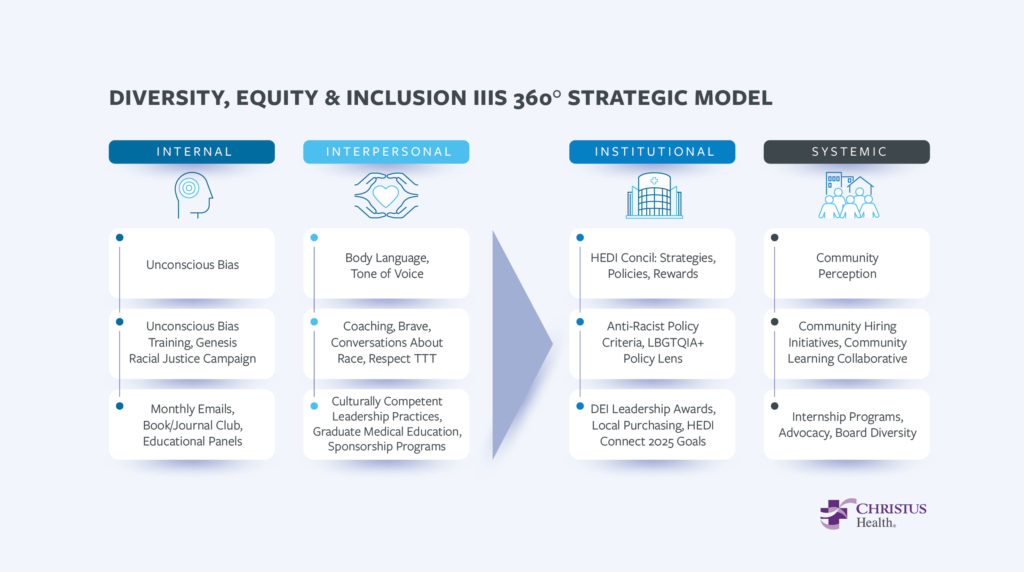
To avoid a reactionary approach to DEI problems, Pesquera and his team adapted the Diversity, Equity and Inclusion 360 Model, a multi-level framework for sustainable solutions to DEI efforts at the Internal, Inter-Personal, Institutional and Structural levels (Figure 1).
He went through each level in detail, explaining how each program or effort fits into each level: the Leadership Sponsorship Program belongs to the Institutional level, while their community collaboration with over sixty organizations that started in 2021 provides grants for community assessments and improvement plans.
Texas Hospitals first reported in 2020 the CHRISTUS GLINT survey, which measured associate engagement. “We selected a few areas and created the D&I Index which measured: belonging, authenticity, respect, inclusion and voice,” said Pesquera.
CHRISTUS used the Index to identify managers who needed additional training on improving and modeling inclusive behaviors. From that group they focused on a cohort of managers that fell under the 25 percentile of their DEI Index as rated by their associates. “We developed a training component to help these managers understand how they’re being perceived and grow in showing more inclusive behaviors,” said Pesquera, “We saw a 5% increase in their scores over three pulses.”
Dr. Mullen added that hospitals can also strengthen ties with community colleges and technical colleges to support developing a diverse workforce.
In the end, Cotton said diversity, equity and inclusion work takes time to see and experience sustainable change, “and that’s really what we’re trying to accomplish.”
