In December 2019, we began hearing murmurings of a novel coronavirus in Wuhan, China. By January 2020, three major airports in the U.S. were screening passengers coming in from Wuhan. Even after the U.S. confirmed its first case in Seattle, we could never have guessed that this novel virus would be so widespread.
As the situation in Wuhan worsened, the Centers for Disease Control and Prevention began to evacuate American citizens from China. Evacuees flew to military bases across the country to quarantine for 14 days. The first group of evacuees arrived at Lackland Air Force Base in San Antonio on Feb. 7. By Feb. 13, one of those evacuees had tested positive for COVID-19.
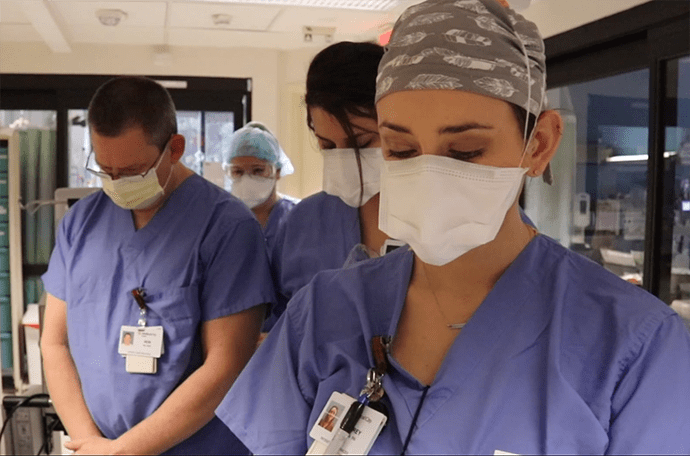
Brian Quinn, a chaplain at Medical City Healthcare in Dallas, has spent countless hours at the bedside of patients. He also provides comfort for our Medical City Healthcare colleagues – rounding on them daily to provide spiritual support and prayers.
Research and Planning Begins
By the end of February, Texas’ health leaders began to plan for scenarios that could unfold as the virus made its way across the U.S. and to Texas.
The Texas Hospital Association began to convene hospitals on calls with the Texas Department of State Health Services to discuss the state of the disease, infection control protocols, preparedness measures, personal protective equipment and other issues.
Hospitals began to implement patient and visitor screenings and coordinate response efforts with nearby hospitals. At this point, the CDC was overseeing all testing – sometimes taking a week for results. Hospitals worked with their local health departments to determine if potential cases needed testing.
“This virus is probably with us beyond this season, beyond this year. I think the virus will find a foothold, and we will get community-based transmission.”
Robert Redfield, M.D., CDC Director, Feb. 13, 2020

Staff at the Hendrick Regional Laboratory celebrate the first internal run of COVID-19 tests at Hendrick Medical Center in Abilene.
The First COVID-19 Case Comes to Texas
On March 4, Houston reported the first confirmed COVID-19 case outside of the evacuees at JBSA Lackland. Texas health officials linked the first cases back to passengers returning from a river cruise in Egypt.
Soon, COVID-19 began spreading to other parts of the state. By March 9, DSHS confirmed community spread. Local authorities started suspending large events – such as the Houston Rodeo, SXSW among others. Public health officials advised older Texans and those with pre-existing conditions to stay home.
On March 11, the World Health Organization declared COVID-19 a pandemic. With cases in over 114 countries and around 4,000 deaths, COVID-19 became the first coronavirus to lead to a pandemic. Two days later, Gov. Greg Abbott declared a state of disaster for all Texas counties.
“One of the greatest challenges ahead is to make sure that the burdens of COVID-19, and our response measures, do not fall on people in society who are vulnerable because of their economic, social or health status. Policymakers must ensure affordable access to testing. Control efforts will be less effective if some fail to seek appropriate diagnosis or care due to high out-of-pocket costs or copays.”
An Open Letter to Vice President Mike Pence and Other Federal, State and Local Leaders from Public Health and Legal Experts in the United States, March 10, 2020

Hector Sanchez, Harris Health Ben Taub Anesthesia Technician Supervisor, shows anesthesia staff members how to use a custom-made protective box while intubating or performing surgical procedures on COVID-19 positive patients. Hector along with Ben Taub Facilities Engineer, Elvis Alavarez partnered on building the large customized protective box to ensure staff’s safety.
Texas Declares a State of Disaster
On March 19, Abbott issued an executive order limiting public gatherings to 10 people, closing schools, prohibiting visitors to nursing homes and limiting bars and restaurants to take-out. The original executive order was to last through April 3, 2020.
On March 22, Abbott made an executive order banning hospitals from performing elective procedures. On March 31, Abbott issued a stay-at-home order urging Texans to remain at home unless participating in an essential activity. Schools would also remain closed for the rest of the school year.
“Hospitals are always ready for emergencies, but COVID-19 will tax the system. That’s why it’s critical we get assistance with the resources we need. The additional production of masks, respirators and ventilators that the U.S. government is pushing for is vital. But this is half the battle. People must follow the rules to protect themselves and our health care workforce.”
Ted Shaw, President and CEO, THA, March 20, 2020

After San Antonio’s Methodist Hospital received its first COVID-19 patient, the Labor and Delivery team quickly collaborated to become the first hospital in San Antonio to offer curbside COVID-19 testing for all maternal patients who were to deliver their babies at the hospital.
Hospitals Prepare Their Most Important Resources
With COVID-19 cases spiking, hospitals began making plans to keep their facilities well-staffed. With non-essential medical procedures canceled, hospitals reassigned many health care providers to departments that needed them most, such as ICUs and emergency departments.
Abbott loosened and waived licensure requirements, allowing out-of-state physicians to practice in Texas, helping retired nurses return to the workforce and enabling student nurses to begin working early. According to the Texas Board of Nursing, more than 700 nurses had reactivated their licenses by April 18.
As the pandemic unfolded, health care providers began using technology to care for patients inside and outside the hospital. Telehealth took off to allow for a way to treat patients safely.
“In this arena [the national distribution of hospital supplies], we have to have an excess capacity for events exactly like this, treating it like a national health security issue, just like we would with military supplies to defend the nation. This is a version of protecting the nation.”
Paul Biddinger, M.D., Director of Massachusetts General Hospital’s Center for Disaster Medicine, April 29, 2020

Staff at Methodist Hospital Stone Oak in San Antonio found innovative ways to celebrate patients’ birthdays.
New Therapeutics Bring Hope
For the first several months of the pandemic, there were no therapeutic medications available for severe cases. By May, Gilead’s Remdesivir had shown promise in early trials in speeding up recovery time among hospitalized COVID-19 patients. DSHS began distributing the state’s allocations to hospitals.
“The Lone Star State continues to prioritize the health of our fellow Texans and ensure that medical providers across the state have the supplies needed to respond to COVID-19. I am grateful to our partners at the U.S. Department of Health and Human Services for providing these cases of Remdesivir to communities across the state of Texas. Texas will continue to act swiftly to provide for our hospitals, secure treatment for patients, and slow the spread of COVID-19.”
Gov. Greg Abbott, May 26, 2020
The Summer Spike Begins
In June, COVID-19 spread outside big cities and was surging across the state. Even so, Texas moved forward with the third phase of the reopening plan – with restaurants permitted to increase capacity to 75% and nearly all businesses allowed to operate at 50% capacity.
Models and data accurately predicted that cases would continue to rise. By June 23 Texas was averaging 5,000 new COVID-19 cases each day. As cases climbed, Texas hospitals shined. Health care heroes continued to scrub in daily and care for a surging number of patients.
As cases continued to spike, Abbott reversed the state’s reopening by again closing bars and reducing restaurant capacity. By July, Abbott began deploying military resources to assist in the state’s hardest-hit areas.
“Think of hospitalizations as that part of the iceberg that you can see that is above the water. Below the water are all the people who are sick but that are not yet in the hospital. The iceberg below the water is far greater than the iceberg above it, and a small increase in hospitalizations indicates a larger increase in illness.”
Clay Jenkins, Dallas County Judge, June 15, 2020
Masks Become the New Normal
Abbott issued an executive order on July 2 requiring Texans to wear masks in public. The mask mandate was met with criticism from some members of the public.
Many large cities and counties already had local mask mandates in place. Earlier in the pandemic, Abbott had blocked local governments from requiring masks. But he clarified that local governments could require businesses to mandate customers wear masks.
“I wish everybody would wear a face mask when they go out. We know that, with two people who have masks on, transmissions’ incidence goes down considerably. I don’t understand why people don’t want to protect each other and protect themselves, especially in the face of everything that’s happening.”
Belinda Metts, RN, Nurse Manager, Houston Methodist Hospital, July 10, 2020

Misha Turner, BSN, RN, CCRN, CA-SANE, a nurse at Texas Health Resources, says working with COVID-19 patients was initially scary. But that over time it’s gotten easier. It’s stressful, she said, because of the uncertainty, but observes that it’s a new normal.
Texans Continue to Lose Health Insurance
According to a Families USA study, job loss stemming from COVID-19 stripped health insurance from an estimated 659,000 Texans between February 2020 and May 2020. In Texas, 29% of adults under 65 — about 4.9 million people — were estimated to be without health insurance in May 2020, the highest uninsured rate of all states.
Public health experts, doctors and elected officials feared that the lack of health care coverage for millions of Texans could complicate efforts to contain COVID-19. The Trump administration eased rules to allow up to 120 days for laid-off workers to sign up for COBRA.
“Even before the pandemic, the cost of care provided to people without insurance in Texas hospitals amounted to more than $7 billion a year. As we look at COVID-19 going forward, it does make the case that we have to look at addressing health coverage. Federal relief money will be directed to health care providers in the coming months. Long term. However, this is unsustainable for Texas hospitals. If unaddressed, this financial burden on hospitals could lead to future cuts and possibly closures.”
John Hawkins, Senior Vice President of Advocacy & Public Policy, THA, July 28, 2020

El Paso Children’s Hospital held their second annual NICU Reunion virtually.
Inequities in Health Care Come into Focus
Over the summer, national protests against racism and police violence laid bare our nation’s inequities in health care and society. With racial inequities at the forefront, new data showed a disproportionate amount of Black and Latino Texans with COVID-19.
According to an analysis from Johns Hopkins University in July, in counties where most residents are Black, the death rate climbed to 3.5 times the national average. DSHS also released data in July showing that while Hispanic Texans make up about 40% of the state’s population, they made up 48% of the state’s COVID-19 cases.
“We are currently facing a critical situation where some of our communities are suffering. We need to do everything to overcome these disparities. But hopefully, this COVID-19 situation has brought out something that we should have been tackling all along — how to overcome these chronic health disparities that our communities suffer.”
Jamboor Vishwanatha, Director, Texas Center for Health Disparities at the University of North Texas Health Science Center, July 30, 2020

Caregivers at Texas Health Fort Worth celebrate with Luis Pamones as he is discharged after 56 days in the hospital.
Fears Mount as Back-to-School Approaches
As Texas cases continued to rise, uncertainty about the upcoming back-to-school season. Research shows that children are less likely than adults to suffer from severe COVID-19, but they can spread mild or asymptomatic illness to school faculty and bring the virus home.
In August, Texas Education Agency and DSHS announced they would be tracking cases in public schools starting in September if the virus was still spreading. This transparency from districts would allow parents to make decisions about in-person learning.
“We know that many families are going to be nervous, and if they’re nervous, we’re going to support them 100%. But if they want an on-campus instructional experience, we want to make sure that we’re offering that throughout the school year.”
Mike Morath, Texas Education Agency Commissioner, Aug. 7, 2020
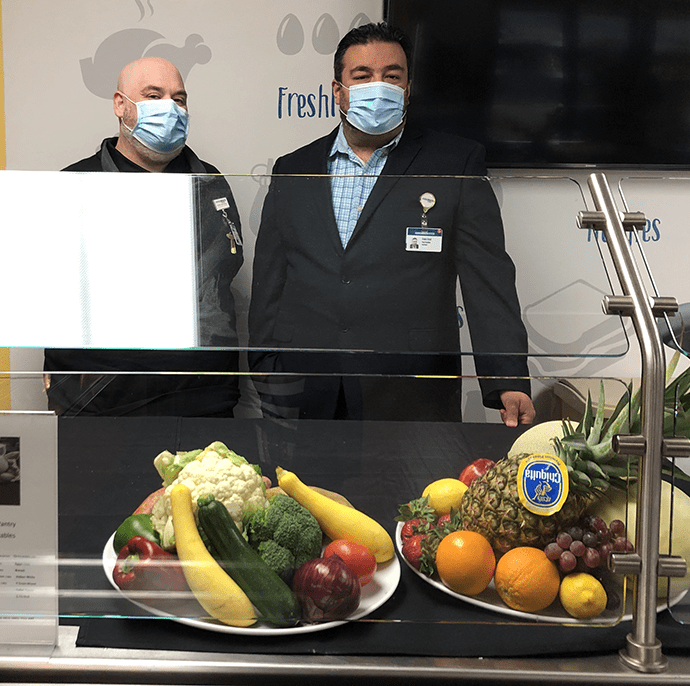
Harris Health System Lyndon B. Johnson Hospital recognized that many of the frontline staff were having challenges getting groceries due to their long hours. They opened a market that offers single-serving and family-style pre-packaged meals and fresh produce for staff to take home.
Preventing a Twindemic
Flu season starts in October, and the 2020-2021 flu season overlapped with the ongoing coronavirus pandemic. Health experts began worrying that an outbreak of influenza and COVID-19 would lead to an unprecedented health disaster – a twindemic.
Hospitals braced for impact, worried that two viruses would be competing for the same resources, doctors, nurses and beds. THA launched a public awareness campaign to urge Texans to get their flu shots and reminding them that the safety measures we take to prevent COVID-19 can prevent the flu too.
A record number of Texans getting their flu shot combined with social distancing, masking and good hygiene practices led to a flu season with historically low activity.
“We have a critical advantage to fight the flu, a vaccine. Hospitals must be working in their communities to increase awareness of the importance of the flu vaccination and increase the percentage of Texans who are vaccinated this year.”
Carrie Williams, Chief Communications Officer, THA, Sept. 18, 2020

When a patient at Texas Health Hurst-Euless-Bedford wanted to be baptized before major surgery, Chaplain Jacquetta Chambers got creative. She baptized the patient in the parking lot two days before surgery.
Texas Surpasses One Million Cases
On Nov. 9, 2020, Texas became the first state to surpass one million COVID-19 cases. Cases in the fall were spiking in West Texas, the Panhandle and major cities. Texas set a new daily record at 10,685 cases on Nov. 10.
By Nov. 21, Texas surpassed 8,000 hospitalizations. With Thanksgiving fast approaching, doctors and public health officials urged Texans to keep their Thanksgiving gatherings small to avoid another spike. However, by mid-December, Texas had the fewest number of ICU beds available for patients since the pandemic began.
“Seeing the good data [in late summer] seemed to send a signal that we were in the right direction and we were in the clear. And I think people lost their vigilance.”
Angela Clendenin, Texas A&M University School of Public Health, Nov. 12, 2020
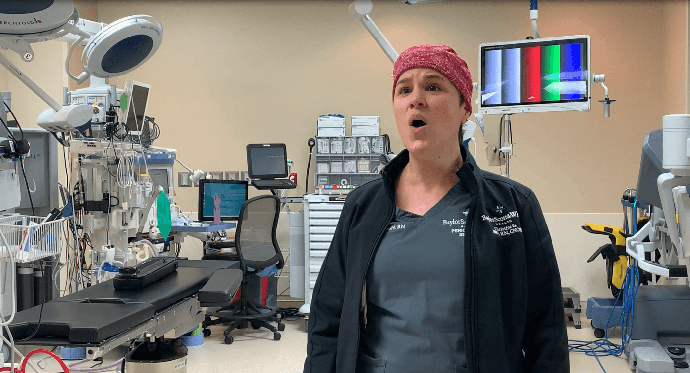
Christine Giammona, BSN, RN is an OR nurse at Baylor Scott & White in College Station who has been using her talents as a professional opera singer during this difficult time to inspire patients and coworkers.
More Therapeutics Come to Texas Hospitals
In November, the FDA issued an EUA for Bamlanivimab, Eli Lilly & Company’s monoclonal antibody therapy. DSHS began making plans to distribute the drug to acute care hospitals across the state.
The medication neutralizes the virus in mild to moderate cases, preventing further developing symptoms into a severe case. A new therapeutic option was welcome news to many hospitals supportive of having the opportunity for a new therapeutic to offer.
But it didn’t come without issue. Bamlanivimab is an outpatient infusion therapy that requires significant space and staff, which was limited. As time went on and hospitals solved logistical problems, monoclonal antibody treatments became a helpful asset for decreasing hospitals’ demand.
“[Monoclonal antibody treatments] are going to be a big benefit to us. Every time we see a new medication, something that looks promising, it’s a step in the right direction, and we’re some step closer to finally getting through this issue.”
Chris Van Deusen, Director of Media Relations, DSHS, Nov. 15, 2020

Hospitalists at Guadalupe Regional Medical Center continue to serve their community.
Mental Health Matters
As the pandemic raged on, health care workers began feeling the mental health impacts. Physician and nurse burnout were already problems – COVID-19 only exacerbated the issue. Almost 64% of the U.S. physicians surveyed by Medscape in 2020 said the pandemic had intensified their sense of burnout.
THA used social media and other messaging strategies to encourage members of the public to support health care workers. THA also released information on techniques that health care providers can use to protect their mental health as they continue to combat COVID-19.
Hospitals across the state continued to support their staff members by acknowledging and celebrating their strength, bravery and knowledge.
“COVID-19 brings significant stressors and is perhaps the greatest challenge in our careers. We all need to look out for each other. When we have a challenge with a patient, we call for help. As physicians and nurses, we need to do the same if we see that one or more of us face significant stresses. We need to know that it’s okay to ask for help.”
David Callender, M.D., CEO, Memorial Hermann Health System, Dec. 11, 2020
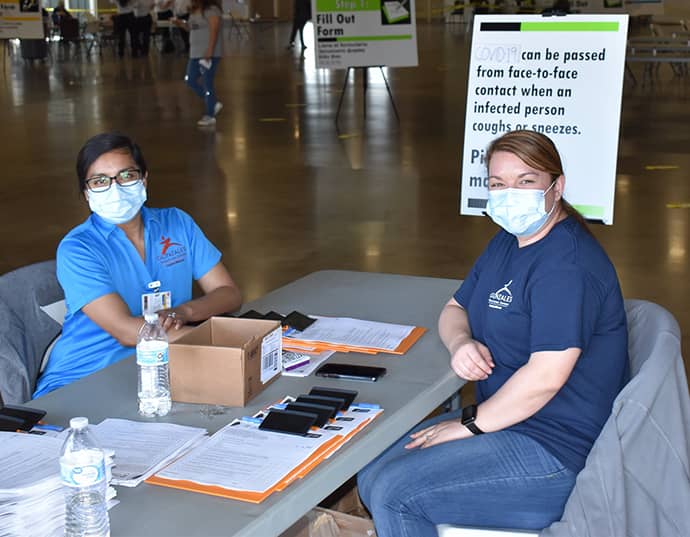
Gonzales County Emergency Management, Gonzales County Officials, City of Gonzales Officials and Gonzales Healthcare System held a mass vaccination clinic at the JB Wells Expo Center. They successfully vaccinated 400 individuals.
Vaccines Arrive in Texas
Christmas came early in 2020, as Pfizer vaccines began arriving to hospitals and into the arms of Texas’ frontline heroes on Dec. 14. DSHS made it a point to prioritize hospital staff directly working with COVID-19 patients in receiving the vaccine.
The Pfizer vaccine received emergency use authorization by the Food and Drug Administration on Friday, Dec. 11, and a second vaccine manufactured by Moderna quickly followed, receiving emergency use authorization one week later, on Dec. 18.
On Jan. 14 – one month after the first doses arrived – Texas became the first state in the US to administer one million doses.
“Seeing the first doses of vaccine arrive in Texas is an important milestone signaling that a return to our way of life is within sight. We cannot stop short of the finish line. This hope should lift our spirits and strengthen our resolve to do what we need to end the pandemic.”
John Hellerstedt, M.D., Commissioner, Texas Department of State Health Services, Dec. 14, 2020

With the help of over 700 volunteers, Memorial Hermann administered over 14,000 first doses of the Moderna vaccine in four days at their COVID-19 Vaccine Drive-Thru Clinic.
The battle isn’t over yet, but there is hope on the horizon. Hospitalizations are the lowest they’ve been since the summer surge. Texas has administered over 8 million vaccines – a number that will continue to increase as vaccines have been made available to all adults. One year into the fight and one thing is certain; Texas’ health care workers are true heroes.
