COVID-19 Impact Report
Hospitals pulled Texas through a pandemic. Now, they face skyrocketing expenses and losses. It’s time to pull for them.
Download the Report

Hope & Healing on the Frontlines
Millions of people turned to Texas hospitals for COVID-19 treatment, testing, vaccination and care during the pandemic. Hospitals were ground zero in the state’s defense against a relentless disease that swept the country and changed lives forever. Ever since Texas’ first case of COVID-19 in February 2020, the health care landscape and financial outlook for hospitals have dramatically transformed.
Now, facing skyrocketing expenses and millions in losses, Texas hospitals are in a precarious position.
The impacts of the COVID-19 pandemic are far and wide, resulting in extreme financial challenges for Texas hospitals. Nearly twice as many Texas hospitals are at risk of closure since before the pandemic.
Hospitals pulled Texas through a public health emergency. Now it’s time to pull for them.
Hospitals: Ground Zero
In early 2020, the first case of COVID-19 was confirmed in Texas, sending all sectors of the state’s health care infrastructure into full-blown response mode. The pandemic took doctors, nurses, hospitals, public health officials and others on a painful and seemingly never-ending journey, responding to multiple surges and variants – and witnessing thousands of deaths – as the pandemic wore on. Hospitals were ground zero for life-saving care and an unprecedented vaccine rollout that helped protect countless Texans. Texas hospitals took care of Texans during the pandemic, and now critical resources are needed to stabilize the state’s health care infrastructure.
Answering the Public Health Call
As part of the state’s COVID-19 response early in the pandemic, and amid a rapidly increasing need for COVID-19 hospital care, the Governor’s Office stated in June 2020 that “every Texan who needs access to a hospital bed will have access to a hospital bed.”
Rallying Amid Pandemics

“If you look back centuries, you see that throughout history, doctors, nurses and other health care providers have rallied amid pandemics, wars and natural disasters, and did what they needed to do to care for those in their communities.”
Dr. Marc Boom
President & CEO, Houston Methodist
2021 THA Board Chair
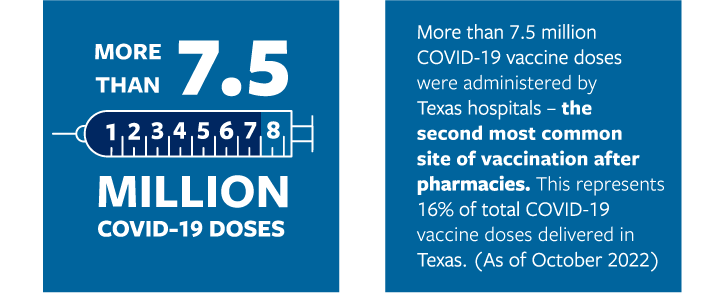
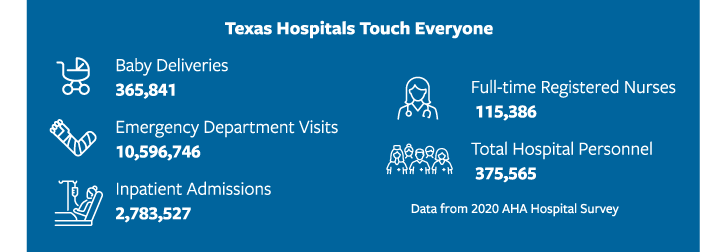
During the pandemic, more than 500,000 COVID-19 patients were admitted to Texas hospitals, taking the system to the brink and creating significant challenges in ensuring patients could get the care they needed. Aside from admitted patients, millions more have been tested, treated, or vaccinated for COVID-19 in hospital outpatient and emergency settings.
As other industries shut down or transitioned to work-from-home arrangements, hospital caregivers showed up, took risks and saved Texans.
Bleeding Along the Way
As cases mounted and hospitalizations climbed, Texas hospitals worked quickly to keep their teams safe. Over time, worries about gloves, gowns and other equipment were replaced by more significant concerns about people – a resource that was precious, finite and susceptible to illness. The country’s health care workforce began shrinking, with severe burnout and shortages ballooning at every health care facility. This year, roughly 500,000 nurses are expected to leave the workforce, bringing the overall shortage to 1.1 million nurses. An entire generation of health care workers was lost to COVID-19 burnout, fatigue, retirements, career changes or illness.
A Halt on Procedures
In March 2020, the State of Texas mandated that “health care facilities shall postpone all surgeries and procedures that are not immediately medically necessary.” While this move was made to help preserve hospital capacity for COVID-19 patients, it left hospitals, particularly in rural areas and in areas with few COVID-19 cases, without the ability to generate revenue. Additionally, delaying certain “non-emergency” services – such as cancer care or preventive procedures – caused health conditions to worsen. As Texans resumed care at hospitals, their conditions had been exacerbated and next-level care was needed, placing additional pressure on the industry.
Mounting a Defense
Amid staff shortages and financial strain, Texas hospitals locked arms with public health to embark on a massive push to vaccinate the unvaccinated. In December 2020, the first COVID-19 vaccines began arriving at Texas hospitals for health care workers who had spent most of 2020 on the frontlines of the pandemic. As the delivery trucks carried vaccines to hospitals, they were greeted by cheers, applause and prayers.
Courage Under Fire

“While most of us were worried about whether the person ahead of us in line at the grocery store might have COVID, uniquely among all professions, team members working in hospitals entered the dragon’s lair every time they were on duty, knowing that a potentially lethal pathogen was present somewhere in that environment. There can be no more powerful definition of courage under fire.”
Dr. John Hellerstedt
Commissioner, Texas Department of State Health Services (2016 – 2022)
Health care workers lined up to be vaccinated, to protect themselves, their patients and their communities. As supplies increased, Texas hospitals scrambled to find the space and staff to vaccinate their communities and administer thousands of doses per day outside their patient base. Texas hospitals answered the call to get shots in arms. They proved to be reliable and critical points of access, enabling the state to vaccinate large numbers of people quickly and efficiently.
Economic Recovery
While launching these unprecedented vaccination efforts, hospitals were grappling with daily record-breaking COVID-19 hospitalizations and fighting to save the lives of the sickest, most vulnerable Texans. Hospitals continued to emphasize personal protection – and protection of their frontlines – as a path toward freedom from this disease.
The state continued to partner with Texas hospitals to execute additional public health response activities during COVID-19, including monoclonal antibody treatments and an ongoing, tiered vaccine rollout. These efforts returned enormous economic benefits to the state. In May 2021, the Texas Comptroller credited vaccine administration – led in many communities by hospitals – for driving the state’s economic recovery as he raised biennial revenue estimates.
Texas Hospitals Came Together
While the full extent of COVID-19’s wrath continues to be calculated, one thing is clear: Texas hospitals worked together to put patients first during one of the most challenging environments ever faced by the health care industry. Together, they fought for what they needed to keep the state safe, including:
- Relief funding
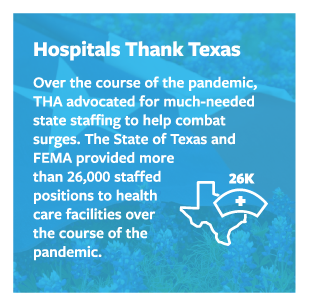
- Staffing
- Vaccine resources
- Therapeutic supplies
- Visitation & screening policies
- Clear, precise masking & social distancing information
- Waivers & flexibilities
- Liability protections
Mission Critical Waivers
The Texas Hospital Association requested nearly 200 federal waivers and state law flexibilities so that hospitals could focus on providing care to an unprecedented number of patients. This includes the suspension of state regulations to permit hospitals to increase their bed counts, treat two patients in a single occupancy room, expedited licensing for health care workers, Medicaid prior authorization exceptions and expanded use of telemedicine.
In addition, THA’s online waiver tracker detailed the category, time period, affected parties and parameters of each waiver or state law flexibility affecting hospitals. THA issued interpretive documents and worked closely with hospitals and state officials to advocate for waiver extensions. These waivers and flexibilities were integral to the state’s response to the pandemic.

A Staggering Financial Toll
Extreme financial pressures on a life-saving industry creates risk for patients and the state’s overall health. The financial strain on hospitals throughout the pandemic has been additive and profound.
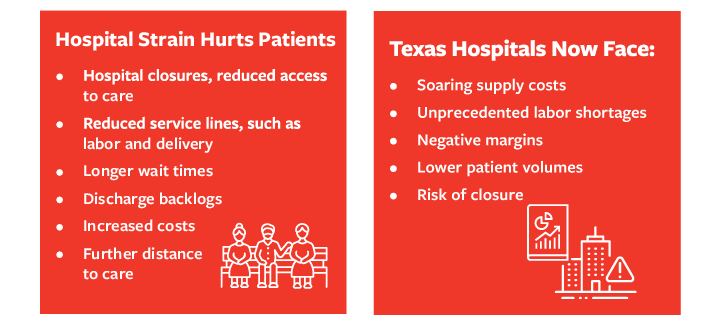
For 2022, nearly half of all Texas hospitals had negative operating margins. Almost one out of every 10 Texas hospitals is at risk of closure.
While state and federal COVID-19 relief was a lifeline for many health care providers, the pressures outpaced the relief, and Texas hospitals are struggling to survive.
Building Blocks of Strain
Early in the pandemic, hospitals moved fast to prepare for mounting hospitalizations and COVID-19 surges. They set up temporary care sites, modified facilities, added equipment, and purchased personal protective equipment, all at a premium amid supply chain woes. Texas hospitals temporarily postponed all non-essential surgeries and procedures to conserve limited supplies of personal protective equipment and increase bed capacity. Then came patient-driven delayed non-emergency care, patient volume losses and soaring labor costs.
All the while, Texas hospitals and other health care providers delivered $3.16 billion in COVID-19 care for the uninsured, and navigated rates that failed to cover the extensive wrap-around care required by a COVID-19-positive patient.
The Numbers Don’t Add Up
The growth in Texas hospital expenses has outpaced any revenue and relief. As a result, Texas hospitals have incurred serious losses relative to pre-pandemic levels – including approximately $3.2 billion in 2022 to date – with no further relief in sight. This represents a 30% reduction in total income across Texas.
For 2022, nearly half of all Texas hospitals had negative operating margins, up from one-third in 2019. While federal support had helped hospitals weather the first two years of the pandemic, 2022 has been extremely difficult, with operating margins 24.1% below pre-pandemic levels in 2019.
Texas hospital expenses are up 20% over pre-pandemic levels. Labor expenses, including contract labor, are 20.9% higher than pre-pandemic levels, while medical supplies are up 8.5% and drug expenses have significantly accelerated over the same time period. As of September 2022, Texas hospitals accumulated more than $3 billion in unreimbursed COVID-19 costs, of which $1.5 billion was unreimbursed staffing. While the State of Texas provided critical staffing assistance, the need outpaced the support as hospitals were vying for staff at rates driven sky-high by staffing companies.
Contract labor expenses have played a significant factor in rising labor expenses. In fact, through August 2022, contract labor expenses for Texas hospitals are $4.9 billion higher than pre-pandemic levels.

Texas hospitals remain in a precarious position as they continue to try to stabilize amid historic workforce shortages and soaring expenses. Simply put, hospital revenue is not covering the cost of patient care. This upside-down way of operating is not sustainable and seriously threatens the ability of hospitals to provide comprehensive care in their communities.
Keeping the Doors Open
The percentage of Texas hospitals at risk of closure has nearly doubled since 2020. Risk of closure has grown for both rural and urban hospitals. While federal stimulus support helped lessen the risk of closure for Texas hospitals in 2020 and 2021, the threat has consistently increased. It’s universally known that hospitals are critical economic – and health – drivers in their communities, and a closure has a ripple effect on jobs and access to health care.
Pervasive shortages in revenue and workforce can lead to reduced hospital service lines, like labor and delivery, surgery, oncology and psychiatric units. Rural and urban hospitals are struggling to afford increasing labor costs, and workforce shortages can severely limit a hospital’s ability to provide next-level specialized care for patients.
Texas data and trends universally show that battle-worn hospitals are emerging financially challenged and depleted of staff and resources as supply costs surge. As a result, the stability of the state’s health care safety net and the financial health of Texas hospitals remain severely threatened. While there is much to rebuild, hospitals hope to return to a new normal in the coming years.
COVID-19 Care Costs More
A single COVID-19 positive patient burdens hospital resources, staff and space, even if that patient is asymptomatic and hospitalized primarily for another reason – such as trauma, stroke, or labor and delivery.
Hospitals launch wrap-around infection control protocols and take special care to protect staff, patients and the community. This care requires tremendous resources at a time when hospital resources are strained. Regardless of whether COVID-19 is the primary reason a person is in the hospital, hospitals must follow clinical standards and governmental regulations for infection control, testing, diagnosing and reporting COVID-19.
Additionally, a COVID-19 infection often worsens the primary illness of patients, sending them to the hospital when they would otherwise be at home. COVID-19-positive patients create risk for hospital staff and require more work, more time and more than twice the resources.
Telehealth: Innovation on the Fly
As Texas hospitals dealt with challenges and dangers amid the pandemic, they moved fast to launch innovative new approaches and technologies to save time, conserve resources and protect people. From virtual visits to new mobile apps to rounding via phone, Texas hospitals tackled new challenges. They launched creative new innovations to conserve masks and other equipment and limit patient exposure during the pandemic.
Texas sought much-needed waivers and flexibilities for certain telehealth-related regulatory requirements so they could prioritize high-quality, safe care during the pandemic. While not a panacea for all access challenges, these efforts have been a game-changer in reaching patients in harder-to-serve areas, providing complete care at home, saving patient travel times and cost.

An Endangered Workforce
The COVID-19 pandemic acutely impacted the people who provide care inside the walls of hospitals. Burnout and fatigue plagued the frontlines, and many health care workers left the field altogether. While health care workforce shortages existed long before COVID-19, staffing costs and other pandemic-related challenges have led to an unsustainable situation that threatens hospitals’ ability to care for patients.
Workforce: Critical Infrastructure
As the state works to rebuild infrastructure, such as power grid capabilities and water resources and address statewide workforce shortages, the No. 1 resource of focus must be health care and the people who provide it. The health care workforce is essential to the state’s infrastructure. Hospitals are open to their communities around the clock, and available to anyone who walks into the emergency room, making health care workforce shortages a true acute issue.
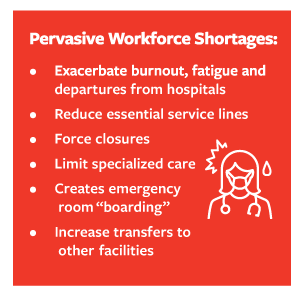
Hospitals are able to provide high-quality patient care because of their skilled and sufficient health care workforce. Skyrocketing labor costs are pushing many providers toward a financial cliff, and limiting the availability of care where hospitals have physical beds available but no staff to provide needed care. As the challenges to find, procure and retain staff continue, the impacts on hospitals’ ability to provide care will continue.
Open Positions, Less Care
Even as the pandemic waned, hospitals continued to scramble to fill positions with permanent staff, alleviate fatigue, prevent workplace violence, implement retention strategies and pivot staff into a new era of health care. Layers of exhaustion and burnout, coupled with mass exits from the profession, have created a health care challenge with regard to workforce – a cumulative effect months in the making.
Longer Stays
Increases in length of stays is being driven by labor shortages in post-acute settings. This leaves hospitals with the inability to discharge patients to lower levels of care in a timely manner. Hospital beds are held by patients who should be discharged, and hospitals incur additional costs from those stays without commensurate reimbursement.
Mounting Labor Expenses
Staffing is roughly 60% of a hospital’s total expenses. Throughout the pandemic, hospitals have seen costs for in-house staffing as well as agency staffing surge to historic levels. Through August 2022, hospital labor expenses are 20.9% higher than pre-pandemic levels — $18.1 billion higher than 2019 due to both higher staffing and contract labor expenses.
Travel Nurses
Large numbers of nursing staff left hospital employment to work as travel nurses. Costs for travel staff were at least double in 2021 over 2020. Premium rates staffing agencies charge for travel nurses are 150% to 200% of standard hourly rates hospitals pay employed staff. Texas currently has the highest reported demand for travel nurses and travel crisis nurses in the nation. Hospitals are working to lessen their reliance on contract staff, but the workforce shortage means there is still an overreliance on staffing agencies to fill open positions.

A Pipeline Problem, Exacerbated
Long-term workforce challenges existed well before the COVID-19 pandemic, with an aging workforce and shortages of nurse faculty and clinical training sites. The COVID-19 pandemic worsened this years-long pain point faced by the industry. This year, roughly 500,000 nurses are expected to leave the workforce, bringing the overall shortage to 1.1 million nurses. Notably, Texas nursing schools turned away more than 15,700 qualified applicants in 2021 due to a shortage of nursing faculty and clinical education capacity. This shows that we have qualified Texans who want to go into nursing, and hospitals have the open jobs.
Burnout & Emotional Impact
People on the hospital frontlines experienced longer working hours, less time with loved ones and increasingly stressful environments during a time of historic uncertainty and supply shortages. Frontline positions are incredibly physical and taxing even during non-pandemic times, and patient challenges are emotionally challenging for those who have dedicated their lives to patient care. Nurse leaders report that the emotional health and well-being of staff is their top challenge today.
The mental health impacts of living and working in a pandemic have been well documented. Health care workers felt the brunt of this impact over the course of the pandemic as new surges emerged, deaths mounted, capacity depleted and risks on the job remained.
Violence Against Hospital Workers
An unfortunate development since the beginning of the pandemic has been a sharp increase in incidence of workplace violence. Sadly, there is no sign that this trend is reversing. Hospital workers report experiencing extreme physical abuse, including being kicked, punched and bitten, and in extreme cases shootings have occurred inside the walls of hospitals.
Health care workers remain five times more likely than any other type of worker to be physically attacked on the job, according to the Bureau of Labor Statistics.
Recent studies indicate that 44% of nurses reported experiencing physical violence and 68% reported experiencing verbal abuse during the pandemic.
Violence against hospital workers:
- Hurts everyone.
- Damages and traumatizes hospital workers.
- Increases workforce departures from acute care.
- Distracts from patient care.
- Ties up resources.
- Delays urgent care.
- Increases adverse medical events.
- Reduces patient satisfaction.
What Would Alleviate Workforce Issues?
- More state funding for physician, nurse, behavioral health professional and allied health professional training, clinical space, retention and loan repayment programs
- More strategies to support health care workplace safety, retention and workplace violence reduction
- More funding to address increased and unreimbursed staffing costs caused by COVID-19

A Toll on Behavioral Health Infrastructure
During the pandemic, anxiety, depression and suicidal ideation increased. However, the number of people accessing behavioral health care decreased in many areas due to limited capacity, loss of coverage, stay-home restrictions and general concerns about COVID-19. Behavioral health hospitals struggled as demand declined in some areas – and surged in others. And they worked to implement telehealth capabilities to address increases in adverse behavioral health conditions – and manage infectious disease risks in their unique settings.
Fewer Resources
Behavioral health care has long been underappreciated and often stigmatized. Unfortunately, behavioral health services remain difficult to access for many Texans, despite investments from the Texas Legislature and national attention on the issue. Behavioral health care is often reimbursed at lower levels than acute care. Additionally, while all hospitals struggled to find staff during the pandemic, workforce shortages in behavioral health have been a historic problem, particularly with regard to psychiatrists in Texas.
During the pandemic, behavioral health hospitals were largely prohibited from accessing relief funding, personal protective equipment and staffing assistance, compared to other providers, even though they cared for COVID-19-positive patients in their units.
Unique Risks
Behavioral health facilities faced unique challenges with risks for self-harm related to the use of masks and alcohol-based hand sanitizers. They faced social distancing challenges in small-group therapeutic settings as well as challenges with turnover, labor costs and burnout among staff. They faced significant negative impacts on revenue as they paused admissions to manage COVID-19 positive patients and board patients for longer lengths of stay as patients recovered from COVID-19 illness.
Moving Forward
More recently, behavioral health care in Texas has moved toward the front and center due to the stress of a pandemic layered with a turbulent economy. The emerging sentiment now is that mental health is physical health; the mind and body are closely related and work together for overall health. It’s a sentiment that all hospitals – psychiatric, general, and state mental health hospitals – have been pushing for years.
What Behavioral Health Hospitals Need Now
- More state funding for physician, nurse, behavioral health professional and allied health professional training, clinical space, retention and loan repayment programs
- More strategies to support health care workplace safety, retention and workplace violence reduction
- More funding to address increased and unreimbursed staffing costs caused by COVID-19
- More attention on inpatient and outpatient reimbursement rates to ensure bed availability for people in need
Crisis Within a Pandemic
The pandemic was not immune to other crises unfolding across the state. In fact, devastating events such as Winter Storm Uri taxed hospitals like never before. The trauma endured by Texas hospitals was not limited to the pandemic, and these events have and will continue to deeply impact Texas residents’ physical, psychological and financial health.
Triaging Crises
From natural disasters to mass shootings, Texas hospitals come together quickly to respond, triage and save lives. An unprecedented pandemic does not stop this work. Over the course of the pandemic, hospitals were filled beyond their normal capacity with COVID-19 patients.
The Texas hospital industry’s timely and comprehensive response to multiple crises put a bigger strain on its workforce and increased the stress and mental health pressures experienced throughout the pandemic. Helpfully, the state’s top-notch trauma care system includes 305 designated hospitals and receives state funding to support the extensive hospital network.
Winter Storm Uri
In February 2021, amid the COVID-19 vaccine rollout, Texas was hit hard by Winter Storm Uri. This meant hospitals were challenged to care for their COVID-19 patients in addition to patients injured by falls on the ice, patients overdue for dialysis who couldn’t access their normal providers, and patients who presented to the hospital for an acute medical concern but stayed post discharge to take advantage of the heat, as their homes had lost power. The Texas Department of State Health Services estimates that a total of 246 people across 77 counties in Texas died due to the storm.
Uvalde Shooting
Tragically, in May 2022, a lone gunman massacred 19 children and two adults when he entered Robb Elementary School and barricaded himself in the building. Multiple hospitals rushed to care for those seriously injured, many of whom would find themselves in an acute care setting for a series of weeks to undergo surgeries and rehabilitation.
Astroworld Injuries & Deaths
In November of 2021, a crowd surge at Travis Scott’s Astroworld Festival forced Houston-area hospitals to rapidly respond to multiple injuries, many of which turned out to be fatal. In all, more than 300 concert goers received medical care and sadly, 10 people died as a result of their injuries.
Hurricanes
Hurricanes Laura and Delta hit Southeast Texas in the fall of 2020. Hospitals in the wake of the storms were able to stay open though they were marginally damaged. Those facilities took on the additional burden of preparing and responding to the storm by hardening their facilities, overseeing repairs due to high water and wind damage and providing medical care to people who fell ill during the storms.

Cases Climbed, Hospitals Shined
The pandemic evolved rapidly, with new guidance and messaging released almost daily. However, the one constant message that has remained since the beginning of the pandemic is the heroism of our hospitals and health care workers. As cases climbed, Texas hospitals shined, and health care heroes continued to scrub in daily to care for patients.
Heroes Work Here
In the early days of the pandemic, photos of health care workers holding signs that said, “We came to work for you. Please stay home for us,” flooded social media feeds and “Heroes Work Here” signage adorned hospital lawns.
The public’s heightened awareness of the health care workforce prompted hospitals to use social media to encourage the public to support frontline workers and adhere to preventative measures out of care for them. The Texas Hospital Association put out a call for health care heroes, asking the public and our hospital members to submit nominations for exemplary health care workers who made an impact in their hospitals and in the lives of patients.
Hospitals across the state ran similar campaigns, supporting their staff members by acknowledging and celebrating their strength, bravery and expertise amid a global pandemic.
With each surge in cases, THA collected more nominations and stories attesting to the heroism of Texas’ health care workers.
Throughout the pandemic and beyond, content relating to Texas’ health care heroes has garnered millions of impressions across social media and other digital platforms. Texas hospitals remain committed to sharing the stories of the hospitals and health care workers who were there when millions of Texans needed them most.

Hospitals Are Vital to Communities
In good times and bad, in times of health care stability and public health emergency, hospitals remain not only vital to treating the sick and injured, but to the economic and social health of communities as well.
Jobs & Economy
In 2020, as the COVID-19 pandemic threatened both lives and jobs all over the nation, hospitals employed more than 6 million people and bought more than $1 trillion in goods and services from other businesses, ultimately supporting about one out of eight jobs in the United States, according to American Hospital Association data.
Hospitals are vital to the health, well-being and economic strength of their communities. Hospitals are often the largest employers in smaller towns, and contribute to a sense of safety and community. A hospital closure or reduction in service lines can have devastating impacts.
Outside Their Walls
Beyond their healing efforts and keeping the nation in business, hospitals in Texas and across the country stepped up during this difficult societal era, helping their communities well outside hospital walls.
One hospital in Lubbock, for example, launched a program to help educate and vaccinate local homebound patients against COVID-19. Another hospital system, in Fort Worth, deployed a program to reach out to struggling families to connect them to screenings, well-child visits and other needed care. Whether through outreach, vaccinations, meals, mobile units or other assistance, Texas hospitals are vibrant contributors to the health of their communities and support the overall well-being of Texas.
Hospitals Need Your Help
In the face of a relentless pandemic, Texas hospitals suffered extreme losses – employees, revenues, patients, stability. They fought a relentless pandemic and protected the public’s health – and now many are battle-worn, operating in the red or struggling to stay open.
Texas hospitals are asking for your support in the following areas:
- Financial Stability
- Workforce Growth to Fill Critical Open Jobs
- Public Health Resources
- Behavioral Health
- Access to Care & Coverage

About the Texas Hospital Association
Founded in 1930, the Texas Hospital Association is the leadership organization and principal advocate for the state’s hospitals and health care systems. Based in Austin, THA enhances its members’ abilities to improve accessibility, quality and cost-effectiveness of health care for all Texans. One of the largest hospital associations in the country, THA represents more than 650 of the state’s non-federal general and specialty hospitals and health care systems, which employ some 400,000 health care professionals statewide.