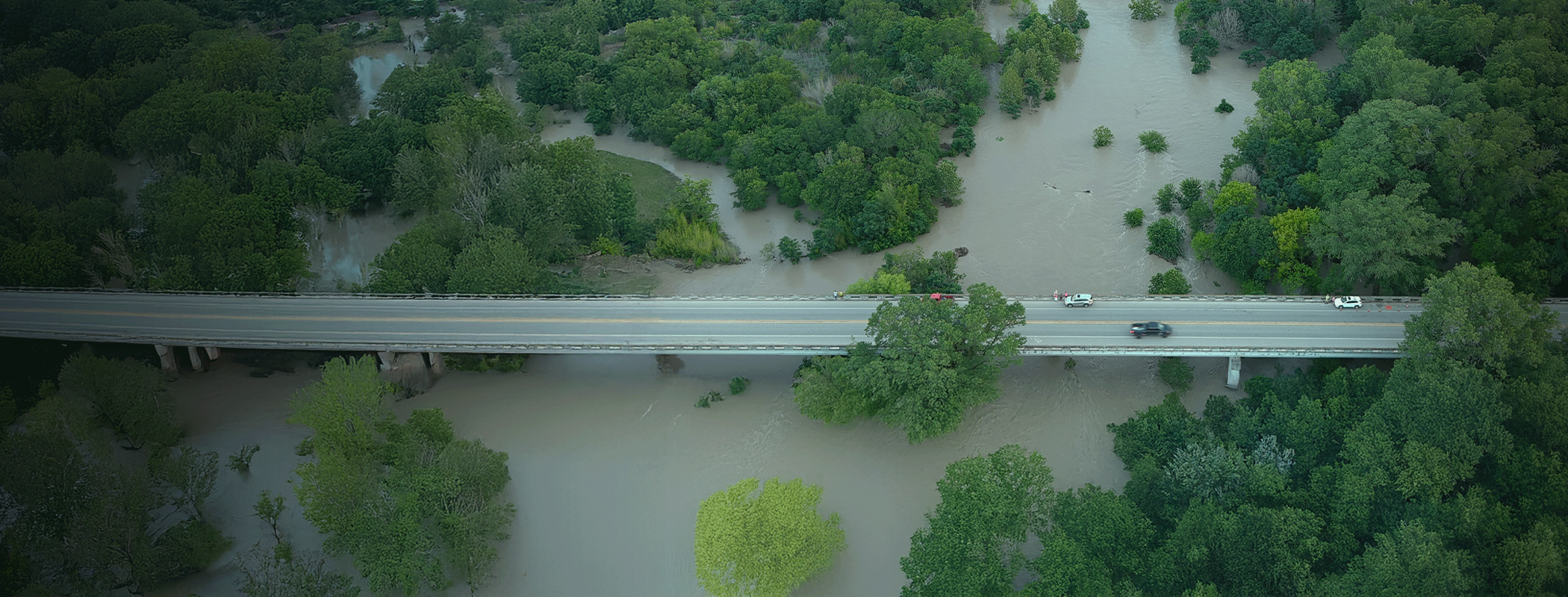
Just one month later, Tim Rye said the whole storm already felt like it was one year ago. But for him – and likely others in Kerrville – routinely driving past the Guadalupe River brings what happened on the Fourth of July back into focus.
“I think driving around town every day, I don’t know that anybody can get home or navigate town without having to drive by the river and just being constantly reminded of it,” says Rye, chief strategic development officer at Peterson Regional Medical Center in Kerrville.
The torrential early July flooding in Central Texas – which killed more than 130 people, became a national news story and thrust disaster preparedness to the forefront of state legislative efforts – was just the beginning of a chain of fast-moving events as local, state and federal authorities hustled to respond to the floods. Peterson Regional was in the thick of the community response during what Rye calls “a surreal period,” and the storm’s impact on hospital personnel was profound.
“Everybody knows somebody who perished or lost something in that flood, for one,” he said. “We had three employees directly affected, losing their houses. Thank God nobody in the hospital perished. But we all knew somebody. So I think trying to keep people motivated to do their work, while the only thing on any of our minds was worrying about loved ones or close friends or church members or whoever, that was hard.”
The Texas Hospital Association is monitoring negotiations and talks on flood relief and disaster preparedness legislation during the current special session of the Texas Legislature, hoping to steer lawmakers toward policy ideas that will make sense for disaster-vulnerable communities and the hospitals that serve them.
“We Did What We Do”
Operationally, Rye says, only Friday, July 4 – the morning that the floods first submerged the river valley – caused a major upset to Peterson’s day-to-day. “Saturday, more or less, we as a hospital were back to normal,” he said. “A lot of our efforts transitioned out into the community Saturday and beyond. Those two weeks after the flood, at least for myself, all I did was flood-related.”
No one at the hospital went to bed on the night of Thursday, July 3, anticipating anything like the storm that unfolded at breakneck speed the next morning. But the early morning hours brought a smartphone weather alert and TV coverage about how quickly the deluge was developing from merely a big storm into something more.
“We called our disaster preparedness [team] and started getting stuff mobilized in the ER,” Rye said. “And I will say that STRAC [the Southwest Texas Regional Advisory Council] was amazing, because they were already mobilized and headed to the area and really helped divert traffic away from our ER that didn’t need to necessarily be there. So that really helped us prioritize patients that were starting to come to the hospital.
“We did what we do. We mobilized the team. We called in extra doctors and nurse practitioners in the ER.”
Normally, Peterson’s emergency department sees roughly 10 to 15 ambulances per day. But on that Independence Day, Rye says, “I can’t remember the exact number; it was over 40 that day. And that was with STRAC diverting [patients] that didn’t need to be there.” The ER ended up with 47 visits that day which were directly flood-related, admitting about a dozen of those patients.
“Most of those admissions were people who had been treading water, holding onto [tree] limbs and stuff, and were just either exhausted or ingested a lot of that water and mostly [were kept under] observation,” he added. “Some of that did turn into some … respiratory illness that we needed to treat and keep an eye on, and they [stayed] in the hospital three or four days for that purpose.”
Along with the assistance from STRAC, many of the worst trauma cases were diverted to San Antonio for treatment, rather than coming through Peterson’s ER. As the aftermath continued, the hospital coordinated the furnishing of needed medical supplies with the Texas State Emergency Operations Center and local volunteer fire departments. Peterson also worked with the Texas Department of State Health Services to administer hepatitis A and Tdap vaccines out in the field for first responders who had been in the contaminated water.
What happened in the field, Rye says, is the “whole story” of the flood: State, local and federal response forces, as well as civilians, stepped up to provide a response unlike any he has seen. “We really played a support role in just trying to keep them functioning,” he said. After that first day, however, the rescue effort was “more or less done,” and the response became a recovery effort.
“I’m proud of our response and what we did in those first few weeks and supporting all those recovery efforts and all those first responders,” he said. “But from a hospital perspective, that first day was crazy and surreal. And after that it was, ‘How else can we help this community even though they don’t need our hospital beds or ERs anymore right now?’”
Moving Forward at the Capitol
Legislation that can help prepare Texas communities for a situation like the floods would be welcome to THA as the Legislature pushes forward this week with its second called session of 2025. The agenda is almost identical to the one from the first special session that began last month, prior to the exodus of Democratic lawmakers meant to stop GOP-spearheaded congressional redistricting. Democrats have returned this week to conduct business in the second special session.
The current agenda includes all of the same flood- and disaster-related items, including focusing on early warning systems, response and preparedness infrastructure, and relief funding specifically for the July storm.
Lawmakers are looking at steps that include:
- Establishment of a Texas Interoperability Council, which would oversee emergency communications and develop a statewide strategic plan, which could include steps like required emergency sirens;
- Forming a new statewide mass fatality rapid response team;
- Supplemental budget funding that would give the governor authority to pursue federal matching funds in the event of a disaster; and
- Training and licensure requirements for county emergency management coordinators.
Benjamin Williams, THA vice president of advocacy & public policy, says the impact on hospitals resulting from steps like these would be downstream.
“Any legislative change that improves disaster response makes it easier on hospitals,” he said. “There’s an argument that sirens would help hospitals by reducing the occurrence of mass events. Getting people to safety reduces the strain on a hospital that’s not set up to help 100 people at a time in an emergency room. When it comes to the second special session, the main issue I can see for hospitals is just the overall disaster preparedness of the state. Texas hospitals are part of that system. So if it gets better, we get better.”
The second special session officially began at noon last Friday, Aug. 15. It can last up to 30 days.
Related articles from The Scope
THA’s 2025 Annual Conference: Advocacy, Achievement and Honoring Excellence
One year and seven months. That’s how much time has…
2025 Newsmakers in Texas Hospitals
Sponsored by Envision Healthcare, THA’s Newsmakers are hospital executives and…
THA’s 2025 Membership Awards
THA would not be the strong voice it needs to…
THA’s 2025 Session in Review: Outcomes for Texas Hospitals
Medicaid talks in Washington, D.C., measles in West Texas and…
National Hospital Week 2025: Appreciation and Awareness
National Hospital Week is a time to celebrate health care…
Women to Know in Texas Hospitals, Health Care and Public Policy
The 89th Texas Legislature is underway and there are a…